What is regenerative medicine?
Regenerative or restorative medicine is an emerging medicine that is rising in popularity, most likely since well-known athletes such as Rafael Nadal and Tiger Woods have benefited from platelet injections. Erik Guay received prolotherapy and Jean-Luc Brassard received stem cells. Promising studies involving stem cells are also being talked about more and more. But, regenerative medicine has actually existed for a very long time…
Regenerative (restorative) medicine is a valuable tool in the treatment of tendon, ligament and joint problems.
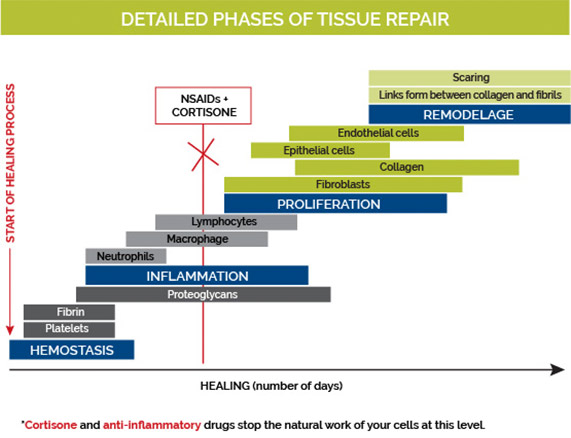
The history of regenerative medicine began with prolotherapy (proliferative therapy). At the time, prolotherapy doctors used irritating substances that were sometimes dangerous (phenol, for example). Over time, doctors realized that the use of dextrose at a concentration of 12.5-15% was sufficient to trigger the inflammatory cascade, essential for tissue healing (see image). Dextrose is a form of sugar given to diabetic patients when they experience hypoglycemia. It is also used in various hospital fluids. Dextrose is a safe and affordable solution that is used regularly in medicine.
In medicine, many studies are funded by pharmaceutical companies. Needless to say, no companies have ever provided resources to research simple dextrose injections. However, even in the absence of funding from the pharmaceutical industry, my colleagues have recently conducted some fine studies internationally, including right here in Canada. Read the studies»
In Quebec, a report issued by INESSS in 2013 stated that prolotherapy was dangerous and that research should stop in this area. It’s important to note that this report is not based on current data and includes toxic substances that haven’t been used in a long time.




Prolotherapy has existed for more than 50 years. It is practiced without complications in all Canadian provinces and all over the world. To date, Quebec is the only one that does not fully recognize its benefits.
It should be noted that it is taught in a Canadian and American association. Harvard Medical School trains physiatrists in prolotherapy.
Prolotherapy is a pillar of regenerative medicine, it is safe, it costs virtually nothing in the public system, and finally, prolotherapy injections with hyperosmolar dextrose are no longer experimental, unlike stem cell injections.
Essentially, regenerative or restorative medicine (dextrose or platelet-rich plasma, and soon stem cells injections) is a great avenue for patients who suffer from chronic pain, osteoarthritis or have tendon or ligament problems.
Hyperosmolar dextrose (prolotherapy) or platelet injections are not a cure-all or a quick fix. They simply represent a very interesting alternative when the patient does not want cortisone, when the conventional approach has failed, or when the patient suffers from different allergies or intolerances to the proposed drugs. None of these therapies (prolotherapy, PRP, stem cells or viscosupplementation) regenerate the cartilage.
At the very least, these therapies slow the deterioration of cartilage and reduce pain, unlike cortisone, which reduces pain, but destroys cartilage.
In regenerative medicine, there are two groups of treatments: biological treatments (PRP and stem cells) and non-biological treatments (prolotherapy, percutaneous needle tenotomy).
nStride – New product!
New treatment for painful knee arthritis
Text to come about nStride.
nStride Brochure
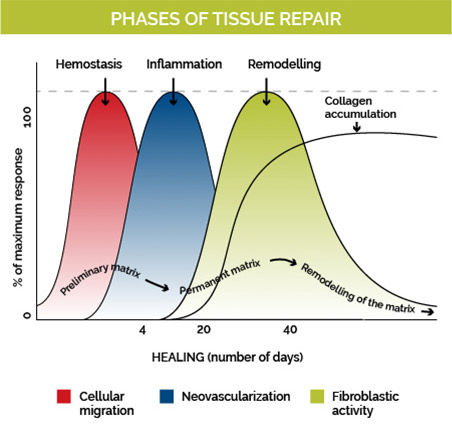
Tissue Repair Phases
Cell migration begins with the injection of dextrose or platelet-rich plasma. For 3 to 4 days, the inflammatory phase dominates. White blood cells and macrophages will clean the inflamed structure (neovascularization) and then send a signal to the construction team (fibroblastic activity) for collagen deposition and repair.
Types of injections available
In regenerative medicine
1- Percutaneous Needle Tenotomy
Percutaneous needle tenotomy or dry needling consists of creating small fenestrations (holes) in the tendons or ligaments using a medium gauge needle.
This procedure causes the injected area to bleed, thus providing the growth factors necessary for tendons and ligaments to heal.
When we use prolotherapy or PRP injection techniques, we indirectly do dry needling.
2- Prolotherapy (Hyperosmolar Dextrose Injections)
Prolotherapy with hyperosmolar dextrose (concentration of 12.5-15%) is an injection composed of dextrose (sugar), lidocaine (anesthetic) and physiologic salin solution. Hyperosmolar dextrose injections stimulate the repair of ligaments, tendons and joints. They also increase their strength. Injections are given every 3 to 6 weeks, and a maximum of six treatments is recommended. The 3-6 week interval is the time required for collagen repair and represents the natural inflammatory process and healing.
The term prolotherapy means therapy that allows to proliferate. Years ago, prolotherapy doctors used several types of irritants to create the inflammation necessary for healing. Some of these irritants are dangerous if injected incorrectly. These dangerous substances are no longer used. Dextrose alone has proved to be effective and above all, safe.
Dextrose is used at a concentration of 12.5-15%. Its concentration becomes irritating to the tissues, thus triggers the healing process (see inflammatory cascade below). Like PRP (Platelet-Rich Plasma) injections, dextrose injections stimulate cell proliferation and self-healing. It is however much less expensive than the PRP.
Advantages of prolotherapy (injections of hyperosmolar dextrose)
Prolotherapy is inexpensive and readily available. It’s very safe, especially when compared to cortisone injections and regular anti-inflammatory drugs. It is regenerative (ligaments and tendons) and not only analgesic. Patients who receive dextrose injections can quickly return to normal activities, in comparison to those who receive PRP.
Download post-prolotherapy injection tips here.
What conditions can be treated with prolotherapy?
- Osteoarthritis of the knee
- Osteoarthritis of the hip
- Muscle tears
- Tendinopathy of the rotator cuff
- Tendinopathy of elbow
- Tendinopathy of the gluteus medius
- Tendinopathy of the hamstrings or adductors
- Patellar tendinopathy (knee)
- Achilles tendinopathy
- Plantar fasciitis (arch of the foot)
- Sequelae of sprain (ankle or knee for example)
Some articles and studies to read
Metaanalyses
Prolotherapy: A Clinical Review of its Role in Treating Chronic Musculoskeletal Pain, Laura M. Distel, MD, Thomas M. Best, MD, PhD
Dextrose Prolotherapy : A Narrative Review of Basic Science, Clinical Research, and Best Treatment Recommendations, Kenneth Dean Reeves, MD, Regina W.S. Sit, MD, David P. Rabago, MD
A Systematic Review of Dextrose Prolotherapy for Chronic Musculoskeletal Pain, Ross A. Hauser, Johanna B. Lackner, Danielle Steilen-Matias, and David K. Harris
Prolotherapy in Primary Care Practice, David Rabago, MD, Andrew Slattengren, DO, and Aleksandra Zgierska, MD, PhD
Securité
Side Effects and Adverse Events Related to Intraligamentous Injection of Sclerosing Solutions (Prolotherapy) for Back and Neck Pain- A Survey of Practitioners, Simon Dagenais, DC, PhD, Oladele Ogunseitan, MPH, PhD, Scott Haldeman, DC, MD, PhD, James R. Wooley, DC, Robert L. Newcomb, PhD
3- PRP – Platelet-Rich Plasma
What is the PRP?
The term PRP stands for platelet-rich plasma. PRP is composed of a high concentration of blood platelets. We produce this high concentration, thanks to the centrifugation of your platelets at the clinic (blood spinning).
How does the PRP work?
Platelets contain growth factors that can stimulate the healing of tissue. The goal of PRP injections is to promote the healing of injured tissue by stimulating your body’s natural healing cascade.
What conditions can PRP treat?
- Osteoarthritis of the knee
- Osteoarthritis of the hip
- Muscle tears
- Tendinopathy of the rotator cuff
- Tendinopathy of elbow
- Tendinopathy of the gluteus medius
- Tendinopathy of the hamstrings or adductors
- Patellar tendinopathy (knee)
- Achilles Tendinopathy
- Plantar fasciitis (arch of the foot)
What is the PRP injection procedure?
The injection appointment lasts up to one hour. You must be accompanied during this procedure. Dr. Ducasse takes a blood sample and puts your blood in the centrifuge at a given speed. This separates your red and white blood cells from your platelets.
Once the centrifugation is complete, platelet-rich plasma is removed from the tube and reinjected into the injured tissue or joint. The procedure is done with ultrasound guidance in a sterile manner.
During the injection, your platelets, now more concentrated, release several growth factors. This release can create inflammation and pain, but that is what allows healing. The whole procedure is done at Dr. Ducasse’s office.
How many treatments will I need?
The response to treatment varies from patient to patient. Some patients require a second treatment, but rarely a third.
A follow-up by phone is planned with Dr. Ducasse, 8 weeks post-injection.
What are the possible side effects ?
There are very few side effects since this is a natural technique where your own blood is used. The most common side effect is increased pain following the injection. This pain can last up to two weeks in rare cases.
The acute inflammation is necessary for the tissue to heal. Sometimes, you may not feel any pain, but the tissue is still healing. The risk of infection and allergy to lidocaine (anesthetic) is very rare. A clot could form or a nerve could be touched.
The risk of deterioration of your condition or the risk of tissue rupture is very low. It is necessary to respect the post-injection recommendations.
What are the recommendations following this intervention?
You should avoid anti-inflammatory drugs (including Advil and Motrin) and cortisone one week before and one week after the procedure. It is useful to start a physiotherapy rehabilitation program two weeks after the treatment.
Sports activities specifically using the treated area are usually not allowed for two to three months depending on your response to the treatment.
When should I consider this procedure?
Usually, this treatment is reserved for cases that have not had satisfactory results with conventional treatment (anti-inflammatory, physiotherapy, cortisone injection, rest, etc.)
On the other hand, with the current knowledge we have of the multiple side effects of cortisone, patients may decide to prioritize the use of regenerative medicine by injecting PRP.
What should I do if I want to receive this treatment?
You must make an appointment with Dr. Ducasse. You do not need a referral ro meet her. She conducts an evaluation during the first interview and tell you if you are a good candidate for the treatment.
Before this first meeting, Dr. Ducasse must receive:
Any radiological report that you consider relevant for the assessment of your condition (magnetic resonance, X-ray, ultrasound, etc.)
By email (unsecured) or by fax (secure): info@dreducasse.com | 514 768-4846
Download post platelet-rich plasma injection tips (PRP).
4- Stem Cells (Dr. Ducasse don’t inject them, more research needs to be done)
Dr Ducasse do not inject stem cells yet because the international medical community still does not agree on the best way to collect stem cells (bone marrow vs. fatty tissue). In addition, there are no markers available for clinical use to identify what types of cells are being removed during sampling. Are these cells still alive or not after being harvested? How many cells are removed? How many cells do we need for optimal performance? Only research laboratories have the ability to accurately identify the injectable cells.
Finally, Health Canada has not yet approved this treatment.
Viscosupplementation
Viscosupplementation (Synvisc One, Cingal, Durolane, Neovisc, Suplasyn, Ostenil, Monovisc, etc.) is hyaluronic acid that is similar to your synovial fluid. This lubricant nourishes your cartilage. Unlike cortisone, there is no maximum number of injections per year. Its cost is high but the effects of viscosupplementation on the joints are excellent. Viscosupplementation has short and long-term positive effects on cartilage protection, thus limiting the progression of severe osteoarthritis.
- Indications: treatment of osteoarthritis
- Contraindications: allergies to chicken or eggs (in the case of Synvisc only)
- Side effects: significant inflammatory reaction at the site of injection within the first three days. (6 injections out of about 100)
Download post-viscosupplementation injection tips here.
